Periodontal disease comprises of a group of diseases affecting the supporting structures of the teeth (periodontium). The most common forms of periodontal disease are caused by bacteria (dental plaque) which reside on the tooth surface, and when left to mature are able to cause an infection of the gums. The end result of this infection is loss of the bone which supports the tooth, which can eventually lead to tooth mobility and tooth loss. The loss of bone support with periodontal disease is in most cases irreversible.
Susceptibility to disease and rate of progression to disease are related to bacterial pathogenicity, individual host responses to the periodontal pathogens, as well as inherent or acquired modifying factors (related to genetic susceptibility and environmental factors). Smoking is by far the biggest preventable risk factor for periodontal disease.

The initial appointment with the periodontist involves a thorough examination and assessment of the gums. This assessment is made through the measurement of the gum pockets (periodontal probing) which will reflect the gum health.
Clinical measurements of gum health will be compared with any radiographic data available, and will enable a diagnosis of your gum condition to be made. A treatment plan will be suggested and discussed with you. As periodontal disease is a chronic condition, commonly no treatment is performed during the consultation appointment.
The main goal of treatment for periodontal disease is to achieve and maintain a healthy functioning dentition for the patient. Given that bacteria are the primary cause of periodontal disease, current periodontal therapy revolves around the physical removal of bacteria and bacterial retentive factors, and the prevention the reformation of bacterial plaque. Advances in our understanding of the pathogenesis of periodontal disease has not changed this basic tenet.
The initial phase of therapy is often termed cause-related therapy, as the bacterial plaque and plaque retentive factors are targeted in this phase of treatment. The objectives of cause-related therapy are to control supragingival plaque levels (to prevent caries and gingivitis) and to arrest periodontal disease and prevent its progression. The following procedures are generally employed to accomplish this:
a. education of the patient to understand the disease process and motivate them to combat the disease
b. providing oral hygiene instruction so that the patient can develop an effective self-performed plaque control regime
c. the removal of plaque and calculus deposits on teeth through scaling and root debridement procedures
d. and the removal of plaque retentive features such as overhanging restorations and ill-fitting crowns
The process of scaling and root debridement (deep clean) is most often performed with the use of hand instruments and ultra-sonic scalers. Depending on the level of severity and treatment needs, this treatment may be performed over one or multiple visits with or without local anesthetic. Severe cases generally require up to four one-hour visits of cleaning. The adjunctive use of antimicrobials is generally not required.
A periodontal review is generally performed three months after the completion of initial phase therapy. This review involves retaking the measurements of the gum pockets and comparing these measures with the initial charting to assess the healing response to the initial treatment. In most situations, this visit will also involve a light clean as well. Your periodontist will then discuss with you your future treatment needs. Periodontal disease is a chronic condition (similar to diabetes mellitus), and hence requires a life long commitment to excellent plaque control and periodic professional maintenance (as is appropriate to your case). The long-term management of periodontal disease always requires regular cleaning with a dental professional in order to prevent recurrence of disease.
Non-surgical therapy is sufficient for most patients, and with ongoing maintenance treatment, they may achieve long term periodontal health. However non-surgical therapy does have its limitations, and sites that remain inflamed and bleeding after the initial phase may require periodontal surgery. Periodontal surgical procedures include: pocket depth reduction procedures; regenerative procedures; crown lengthening; and soft tissue grafts.
The advantage of surgical procedures is that it allows for the improved assessment of root surfaces, and the restoration of periodontal anatomy damaged by periodontal diseases and thus facilitates oral hygiene practices. The decision to perform periodontal surgery is generally discussed with you at the first review appointment (three months after the completion of initial-phase therapy).
Dental implants have become the treatment of choice for the replacement of missing teeth in many situations. Dental implants can be used to support single teeth, multiple teeth (bridgework) or even full arch situations (denture or bridge). Dental implants involve the placement of an implant fixture (a medical grade titanium implant) in the jawbone, following which a tooth (crown) can be placed onto the implant. In this situation, the implant serves as the foundation of the new tooth. In most situations, the surgery for placing a single tooth implant will take less than 90 minutes. As the dental implant relies upon bone for anchorage, where the volume of bone is insufficient, bone grafting procedures may be required.
At Perio Partners, our practitioners are highly trained in the surgical placement of dental implants. We use only the most reputable implant systems and are dedicated to the follow up and long-term care of implants.


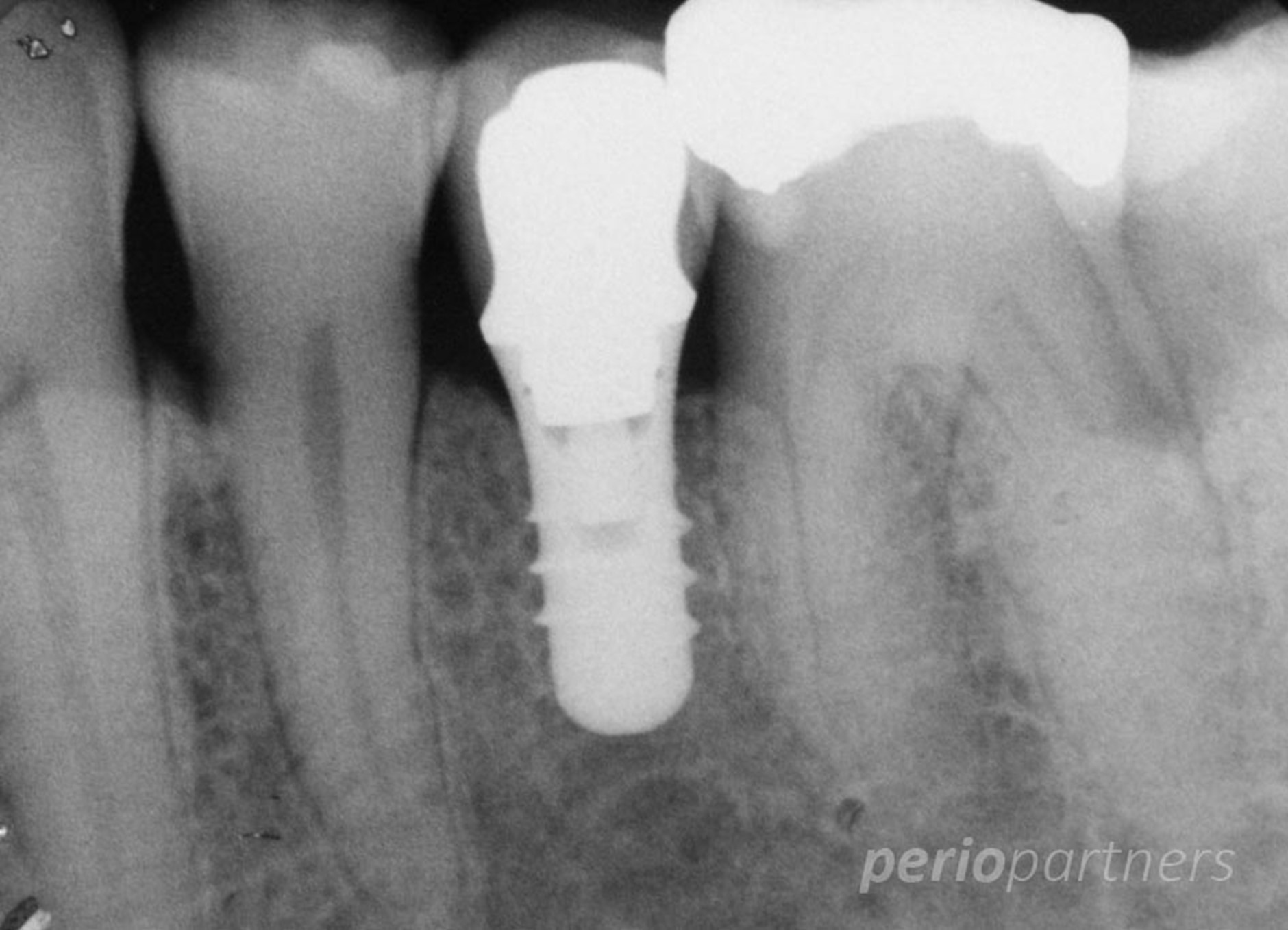
Peri-implant infections, including peri-implant mucositis and peri-implantitis, are challenging complications that periodontists manage due to the complex anatomy of implants and the often aggressive progression of disease. While early stages like mucositis may respond to nonsurgical treatments such as mechanical debridement and antimicrobial therapy, peri-implantitis frequently requires surgical intervention. Surgical approaches allow for access to thoroughly decontaminate implant surfaces, resect or regenerate affected bone, and improve long-term stability. Despite treatment, managing these infections remains difficult, and outcomes can be unpredictable, especially in advanced cases.
Periodontists perform gum grafting to treat gingival recession and improve tissue thickness and aesthetics. The gold standard is the autogenous connective tissue graft, typically harvested from the patient’s palate, due to its high predictability and success in achieving root coverage and tissue integration. However, xenografts (such as porcine-derived collagen matrices) are also used as alternatives, especially when patients prefer less invasive procedures or when donor tissue is limited. While xenografts may offer reduced morbidity and acceptable outcomes, autogenous grafts generally provide superior long-term results.
Diagnosis and management of complex conditions affecting the oral mucosa, temporomandibular joint (TMJ), facial pain, and non-dental oral lesions.
Diagnosis and management of complex conditions affecting the oral mucosa, temporomandibular joint (TMJ), facial pain, and non-dental oral lesions.
Diagnosis and management of complex conditions affecting the oral mucosa, temporomandibular joint (TMJ), facial pain, and non-dental oral lesions.
Diagnosis and management of complex conditions affecting the oral mucosa, temporomandibular joint (TMJ), facial pain, and non-dental oral lesions.
Temporomandibular pain disorders (TMPD) refer to a group of conditions affecting the temporomandibular joint (TMJ), masticatory muscles, and associated structures, often presenting as jaw pain, limited movement, and joint sounds. Oral medicine specialists manage TMPD through a multidisciplinary, conservative approach, focusing on behavioral modification, physical therapy, occlusal splints, and pharmacologic management (e.g., NSAIDs, muscle relaxants, or antidepressants). In more resistant cases, botulinum toxin injections or referral for surgical evaluation may be necessary. Long-term management emphasizes patient education, stress reduction, and habit control, as TMPD is often multifactorial and chronic in nature.
Facial pain can result from a variety of causes, including dental issues, temporomandibular joint disorders (TMD), neuralgias, and neuropathic conditions like trigeminal neuralgia. Oral medicine specialists play a key role in diagnosing and managing these complex pain conditions, often through a comprehensive evaluation that includes medical history, clinical examination, and diagnostic imaging. Treatment approaches vary based on the underlying cause, but may include pharmacologic management (e.g., analgesics, anticonvulsants, or muscle relaxants), physical therapy, occlusal splints, and behavioral therapies for stress or bruxism-related pain. For more refractory cases, botulinum toxin injections or nerve blocks may be used. A multidisciplinary approach is often necessary, involving collaboration with neurologists, pain specialists, and other healthcare providers.
Oral lesions encompass a wide range of conditions, including ulcers, sores, infections, and neoplasms. Common types include canker sores (aphthous ulcers), oral lichen planus, herpes simplex virus infections, and oral cancers. Oral medicine specialists are key in diagnosing these lesions, often performing biopsy, clinical examination, and imaging to determine the cause. Management typically involves topical treatments (e.g., corticosteroids for inflammatory lesions), antiviral therapy (for herpes), or systemic medications (such as immunosuppressants for autoimmune conditions). For suspicious or potentially malignant lesions, a biopsy is performed, and further referrals for surgical management or oncologic care may be necessary. Additionally, specialists provide patient education on prevention, oral hygiene, and lifestyle modifications to minimize recurrence or complications.
Diagnosis and management of complex conditions affecting the oral mucosa, temporomandibular joint (TMJ), facial pain, and non-dental oral lesions.
Diagnosis and management of complex conditions affecting the oral mucosa, temporomandibular joint (TMJ), facial pain, and non-dental oral lesions.
Providing expert dental care with advanced technology in a comfortable and friendly setting. Your smile is our priority!
© 2025 Periopartners. All Rights Reserved
| By Periopartners